|
Neuroscience of Death
When we die, what happens inside our brains? This big question has many answers, and science is helping us understand more. In this note, we look at how the brain works when life ends. In other words, this is about the last part of life and how the brain slowly stops working. Join us to learn more about this important topic in a way that's easy to understand.
When we talk about the end of life, it's important to understand what happens in our brains during this final stage. This can be a complex topic, but let's break it down into simpler terms. Our brain is like the control center of our body, and when it stops working, it signals the end of life. In this note, I will go through some of the key changes that occur in the brain as life comes to an end. I'll discuss how the brain stops getting the blood and oxygen it needs, how this affects the
brain's energy, and the various changes in brain cells and chemicals. I will also talk about how these changes are detected and what they mean for the overall process of death. My goal is to provide a clear and straightforward explanation of this profound and universal aspect of human life
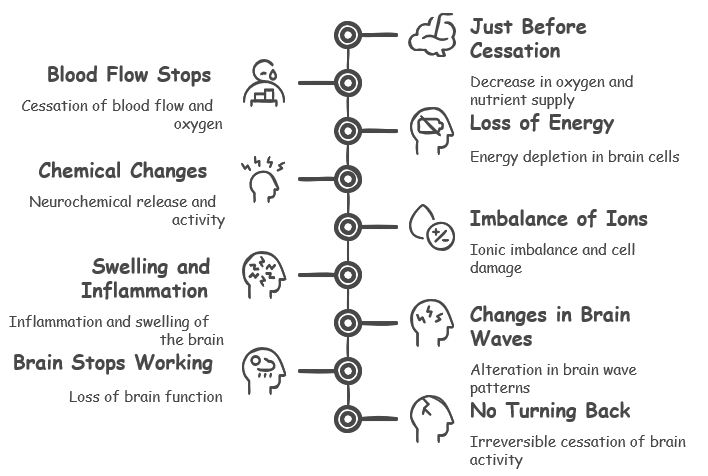
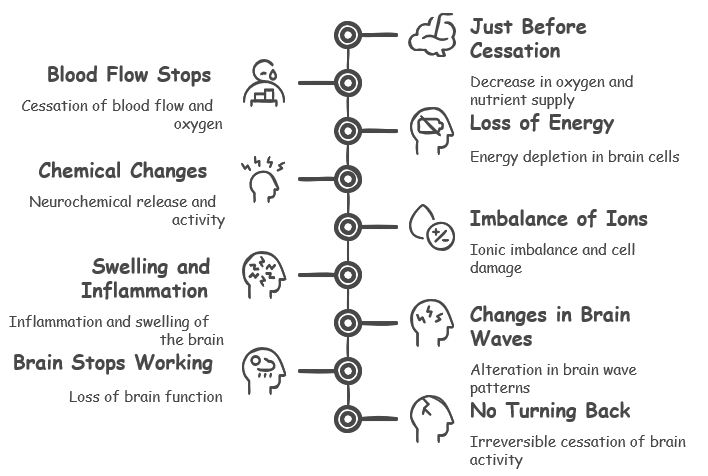
Followings are list of key changes happening during the final stages of our life.
- Just Before Cessation: In the moments leading up to the cessation of blood flow, the brain may experience a decrease in oxygen and nutrient supply due to declining heart function. This can result in subtle changes in brain activity, with potential alterations in consciousness or neurological function. During this phase, the body may attempt to compensate for the reduced blood flow, but these efforts are typically insufficient to maintain normal brain function
- Blood Flow Stops(Cessation of Blood Flow and Oxygen): The main thing that happens when life ends is that blood stops flowing to the brain. This means the brain doesn't get oxygen and other important things it needs. When this happens, brain cells start to die very quickly.
- Loss of Energy(Energy Depletion): Brain cells need oxygen and a sugar called glucose for energy. Without blood flow, the brain runs out of energy and starts to not work properly, leading to the death of its cells.
- Chemical Changes(Neurochemical Changes): As brain cells die, they release different chemicals. These chemicals are usually used for brain cells to talk to each other. But when they're released in this way, it can make the brain very active for a short time before it starts to slow down a lot.
- Imbalance of Ions(Ionic Imbalance): Brain cells have a careful balance of things like sodium, potassium, and calcium. When brain cells die, this balance is upset, which causes more damage to the cells and eventually leads to their death.
- Swelling and Inflammation(Inflammation and Swelling): When the brain dies, it can become swollen and inflamed. This swelling makes the brain's condition even worse.
- Changes in Brain Waves(Brain Wave Changes): As life ends, the brain's wave patterns change. At first, there might be a quick burst of activity. But as the brain gets less oxygen, the faster waves that help with thinking and being awake get weaker. Slower waves take over, showing that the brain is not as active. Finally, there are no waves at all, which an EEG test can show, meaning there is no brain activity.
- Brain Stops Working(Loss of Brain Function): As more brain cells die, the brain can't do its jobs anymore. This includes simple things like reflexes and more complex things like thinking. The brain also stops doing things that keep us alive, like breathing and keeping our heart beating.
- No Turning Back(Irreversible Cessation): After a certain point, the damage to the brain is too much and can't be fixed. This is usually shown by an EEG test that finds no activity in the brain at all. This means that the end of life has truly come.
Just arranging the changes during the death along a time line, it can be aligned as follows.
|
Time Relative to Blood Flow Cessation
|
Neurological Change
|
|
Just Before Cessation
|
Pre-Cessation Changes (e.g., reduced blood flow, oxygen levels begin to drop)
|
|
0-4 minutes
|
Cessation of Blood Flow and Oxygen, Initial Neurochemical Changes
|
|
4-10 minutes
|
Energy Depletion, Continued Neurochemical Changes, Ionic Imbalance
|
|
10-15 minutes
|
Brain Wave Changes
|
|
15-30 minutes
|
Extended Ionic Imbalance and Energy Depletion, Inflammation and Swelling
|
|
30 minutes to several hours
|
Loss of Brain Function, Flattening of EEG
|
|
Several hours to irreversible cessation
|
Irreversible Cessation
|
NOTE : Take this timeline just as a rough estimate, not the exact numbers.
Recently there were several important observations about brain wave changes (EEG) during the course of dying and I found a good review paper like What happens in the brain when we die? Deciphering the neurophysiology of the final moments in life and many articles listed in reference
section. In this sectioin, I will summarize about those
findings.
- Before Death:
- Decrease in Neuronal Activity: There's often a decrease in overall neuronal activity as the brain approaches death. This includes changes in the frequency of neural oscillations.
- Alpha Band Activity: Alpha band activity (8–12 Hz), often related to states of relaxation or idling, might change in its functional significance.
- Gamma Oscillations: Gamma band activity (>40 Hz), associated with consciousness and attention, can show alterations. This wave is associated with higher brain functions like memory, cognition, and attention. Some researchers believe that these changes could be linked to the vivid experiences reported by some people near death, such as seeing a bright light or feeling a sense of peace.
- At the Moment of Death:
- Surge of Oscillatory Activity: Right at the onset of death, especially in cases like cardiac arrest, there can be a surge in gamma oscillations, reflecting intense neural activity.
- Increased Connectivity and Phase-Coupling: This surge is accompanied by increased connectivity across different brain regions and phase-coupling with other frequency bands like theta and alpha.
- After Death:
- Isoelectricity (Flat EEG): Following the surge, the EEG eventually flatlines, indicating a cessation of detectable brain activity. This flatline is the traditional marker of brain death.
- Potential for Resuscitation: Interestingly, the paper discusses the potential for some recovery of brain function if re-oxygenation occurs within a brief window after the onset of isoelectricity.
The process that I mentioned above can be represented in illustration as follows.

Image Source : What happens in the brain when we die? Deciphering the neurophysiology of the final moments in life
Here’s a breakdown of what each stage represents:
- Oxygen Depletion (A): Initially, as the brain begins to experience a lack of oxygen, there's an increase in beta (15Hz) and gamma (40-80Hz) oscillations. This reflects a heightened state of brain activity despite the onset of oxygen deprivation.
- Low Frequency Activity (B): As the brain continues to lose oxygen, the high-frequency activity transitions to low-frequency oscillations. This indicates a significant reduction in brain function and could correspond with the loss of consciousness or active thought processes.
- Isoelectricity (C): This phase shows the brain reaching a state of isoelectricity or a "flat line," where there is no detectable electrical activity. This is commonly associated with brain death, where brain function has ceased.
- Cytotoxicity and Death (D): Following isoelectricity, cell death occurs due to toxic factors released from damaged cells. This stage represents the point of no return where brain cells have been irreversibly damaged and recovery of brain function is not possible.
- Wave of Resuscitation (E): Interestingly, the graph shows a "Wave of Resuscitation" following re-oxygenation, suggesting that if oxygen is reintroduced within a critical time window, there may be a potential (though likely limited) for some brain activities to resume.
Why the brain wave change ?
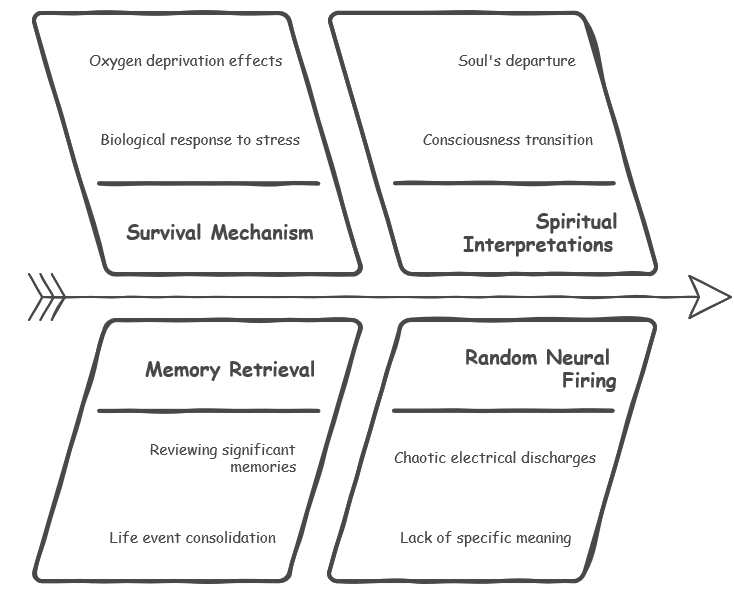
The exact reasons behind these brainwave changes are unclear but there are a few possible explanations. Some researchers believe that the increase in gamma wave activity could be the brain's way of trying to survive the dying process. Others suggest that it could be a mechanism for reviewing important life events or memories. Followings are a little bit of further details :
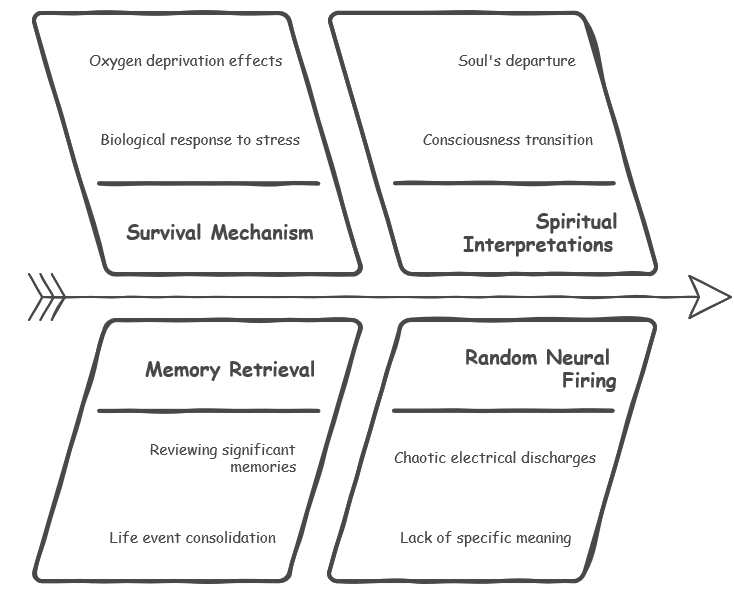
- Survival Mechanism:
- Some researchers speculate that the surge in gamma wave activity, along with other neural oscillations, could be the brain's final attempt to survive. In essence, it could be a biological response to the extreme stress and oxygen deprivation occurring during the dying process.
- This theory suggests that the brain is trying to rally its resources and potentially restore function, even as other bodily systems are failing.
- Memory Retrieval and Life Review:
- Another intriguing possibility is that the brainwave changes facilitate the retrieval of significant memories and life events. This could explain the anecdotal reports of near-death experiences (NDEs), where individuals describe vivid recollections of their past.
- It is hypothesized that the brain might be rapidly reviewing important moments or attempting to consolidate life experiences in its final moments.
- Spiritual or Consciousness-Related:
- Some interpretations delve into more spiritual or philosophical realms. These viewpoints suggest that the heightened brain activity could be linked to a transition of consciousness or the soul leaving the body.
- While this remains speculative and difficult to scientifically investigate, it's a perspective that resonates with many people's personal beliefs about death and the afterlife.
- Random Neural Firing:
- A more pragmatic explanation is that the brainwave changes observed during dying are simply random and disorganized neural firing. As the brain loses oxygen and function, it's possible that these patterns are just chaotic electrical discharges with no specific meaning or purpose.
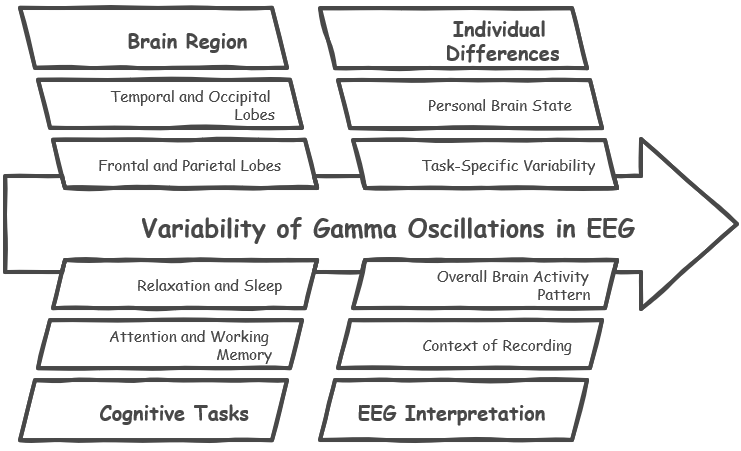
Is gamma oscillation associated with any specific probe position ?
Gamma oscillations in the brain are not strictly localized to a single probe position in the 10-20 EEG system. However, certain brain regions tend to show more pronounced gamma activity during specific tasks or states.
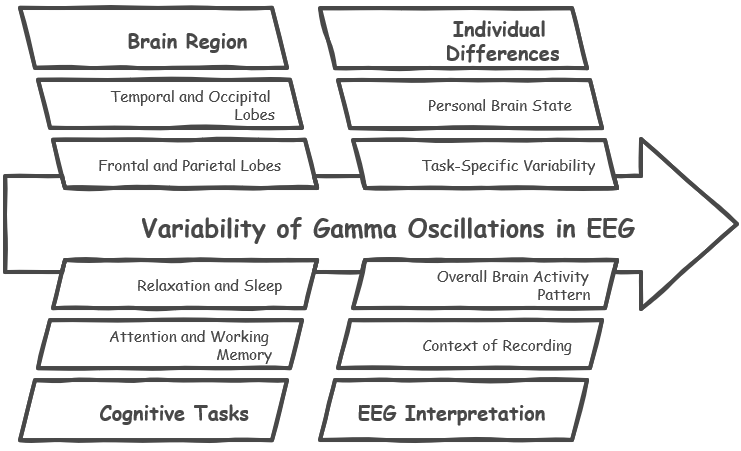
Common Regions Associated with Gamma Oscillations:
- Frontal and Parietal Lobes: These regions are often associated with higher cognitive functions like attention, working memory, and perception. Gamma oscillations in these areas have been linked to active information processing and conscious awareness.
- Temporal Lobes: Gamma activity in the temporal lobes has been implicated in various processes, including auditory processing, memory formation, and emotional regulation.
- Occipital Lobes: Gamma oscillations in the occipital lobes are primarily associated with visual processing and perception.
Dynamic Nature of Gamma Oscillations:
- It's important to note that gamma oscillations are not static phenomena. Their presence and intensity can vary depending on the individual, the specific task being performed, and the overall state of the brain. For example, gamma activity might increase in certain regions during focused attention, while it might decrease in others during relaxation or sleep.
Interpreting EEG Data:
- While specific probe locations can provide valuable information about the distribution of gamma activity, it's crucial to interpret EEG data in the context of the overall brain activity pattern and the specific conditions under which the recording was made.
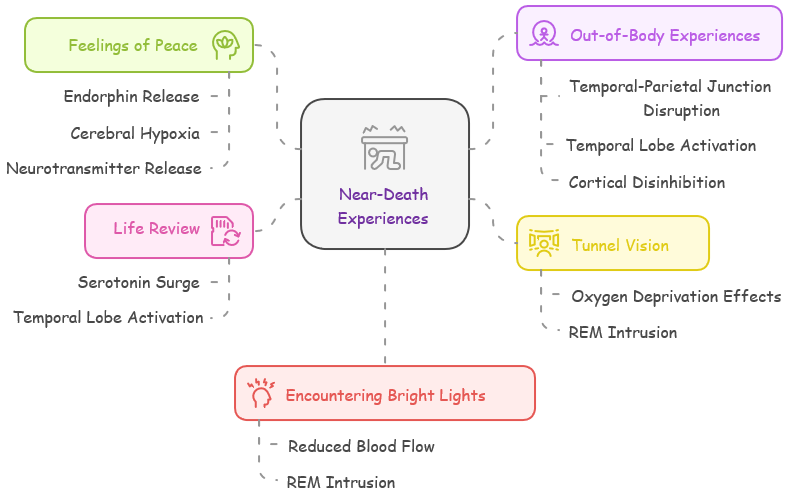
Near-death experience (NDE) is a phenomenon where people on the brink of death report extraordinary events. They tell of feelings of peace, seeing bright lights, or even watching their life unfold before them. These tales have been told throughout history, but only now are we starting to piece together the puzzle.
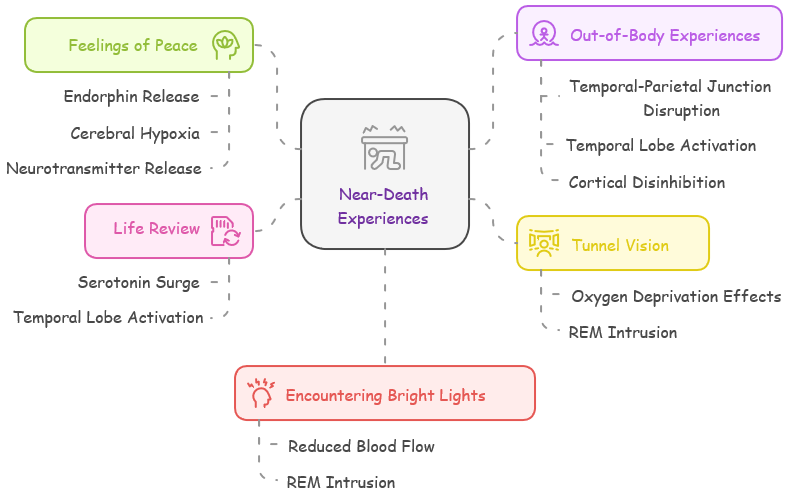
Followings are a list of common experiences (NDE) that are reported and possible neurological background :
- Feelings of Peace: The brain's response to extreme stress may include an endorphin release, which can induce a sense of calm. These naturally occurring opioids are pain-relievers that can create a feeling of euphoria.
- Cerebral Hypoxia: Reduced oxygen to the brain can trigger the release of endorphins, natural painkillers and mood elevators, leading to a sense of calm and well-being.
- Neurotransmitter Release: The release of dopamine and serotonin can also induce feelings of pleasure and tranquility.
- Out-of-Body Experiences(OBE): Such sensations could be due to disruptions in the temporal-parietal junction, the region that integrates sensory information and contributes to body awareness. Anomalies here might lead to a disconnect between the self and the body. These could relate to altered EEG patterns in the temporal-parietal regions, reflecting disrupted body awareness.
- Temporal Lobe Activation: Disruptions or abnormal activity in the temporal lobe, a region responsible for sensory integration and self-perception, can create illusions of floating outside one's body or observing oneself from a distance.
- Cortical Disinhibition: The breakdown of inhibitory mechanisms in the brain's cortex could lead to distorted perceptions of the self and the environment, contributing to OBEs.
- Tunnel Vision: Oxygen deprivation (hypoxia) affects the visual cortex and can cause tunnel vision or light perceptions, often described in NDEs. Hypoxia can produce characteristic EEG changes, such as slowed or attenuated brain wave patterns, particularly in the visual cortex.
- Cerebral Hypoxia: Oxygen deprivation can affect the retina and visual cortex, leading to peripheral vision loss and the sensation of a narrowing tunnel of vision.
- REM Intrusion: During REM sleep, the brain generates vivid imagery, and REM intrusion during wakefulness could produce the tunnel vision experience.
- Life Review: Serotonin, a neurotransmitter involved in memory and mood, may be released in large quantities during stress, potentially leading to the life review phenomenon where past memories rapidly resurface. Serotonin surges may be detectable as heightened EEG activity due to their role in memory processing.
- Temporal Lobe Activation: This region plays a crucial role in memory processing, and its activation could trigger a flood of past memories, creating a life review experience.
- Neurotransmitter Release: The release of certain neurotransmitters might facilitate memory recall and contribute to the vividness of the life review.
- Encountering Bright Lights: Reduced blood flow in the eye can impair the retina's function, possibly leading to the experience of seeing bright lights or tunnel-like visions.
- Cerebral Hypoxia: Oxygen deprivation can affect the optic nerve and visual cortex, leading to hallucinations of bright lights or flashes.
- REM Intrusion: The dreamlike imagery generated during REM sleep can include bright lights or celestial scenes.
How just the sense of OBE(Out of Body Experience) looking down its own body and surrounding area can describe exactly what had happened which would require physical observation ?
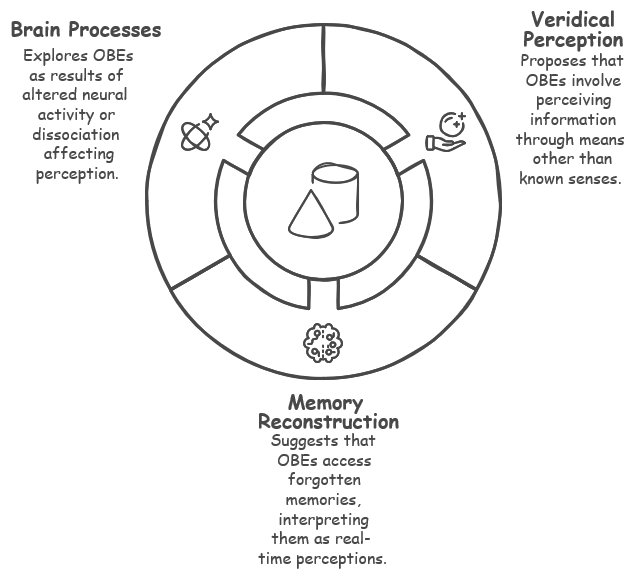
The phenomenon of individuals accurately describing events or surroundings during an out-of-body experience (OBE) while seemingly lacking physical access to that information presents a fascinating puzzle. Several hypotheses attempt to explain this phenomenon:
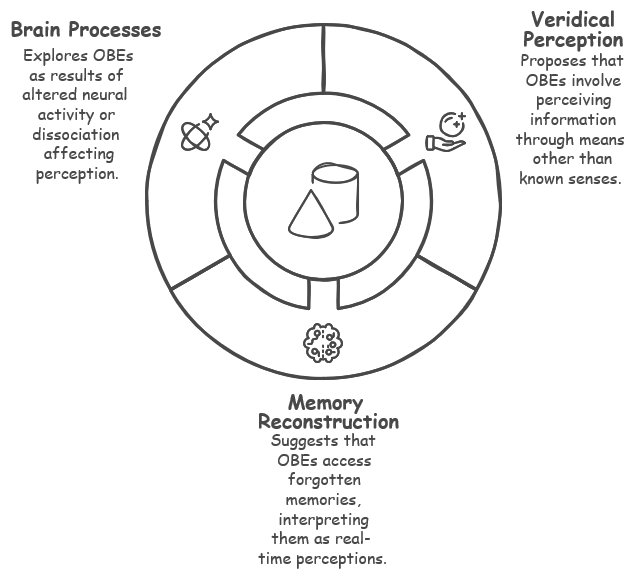
- Veridical Perception:
- Extrasensory Perception (ESP): Some propose that OBEs involve a form of ESP where individuals perceive information through means other than the known senses. This could include clairvoyance (seeing distant objects), clairaudience (hearing distant sounds), or telepathy (communicating with others mentally).
- Subtle Energy Fields: Others suggest that OBEs involve accessing a subtle energy field that contains information about the physical world. This field could be perceived during the OBE, providing access to otherwise unavailable information.
- Memory Reconstruction:
- Cryptomnesia: This theory posits that individuals subconsciously access memories or information they had previously encountered, but forgot they knew. During an OBE, these memories could be retrieved and interpreted as real-time perceptions.
- Suggestibility: Some suggest that individuals may be susceptible to suggestion during an OBE, unconsciously incorporating information from their surroundings or expectations into their experience.
- Brain Processes:
- Altered Neural Activity: OBEs could be a result of altered neural activity in the brain, creating a distorted sense of self and perception. This could lead to the brain generating sensory information based on internal models and memories, which may appear to be veridical.
- Dissociation: OBEs might be a form of dissociation, where individuals experience a disconnection between their consciousness and their physical body. This could allow for a different mode of perception that seems to provide access to external information.
While anecdotal accounts of veridical OBEs are abundant, scientific evidence remains inconclusive. Several studies have attempted to investigate this phenomenon, but methodological challenges and the subjective nature of OBEs make it difficult to draw definitive conclusions.
The mechanisms behind veridical perception during OBEs, if they exist, remain poorly understood. Further research is needed to explore the various hypotheses and determine the extent to which OBEs can provide accurate information about the physical world.
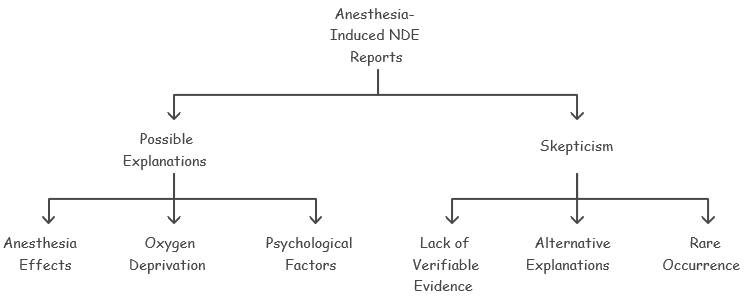
Is there any case where a person who woke from anesthesia and report NDE(near death experience) ?
There have been anecdotal reports of people who, upon waking from anesthesia, describe experiences that could be classified as near-death experiences (NDEs). These experiences often involve feelings of peace, out-of-body sensations, seeing light, or encountering deceased loved ones. However, it's important to note that the scientific community is divided on the interpretation of these accounts.
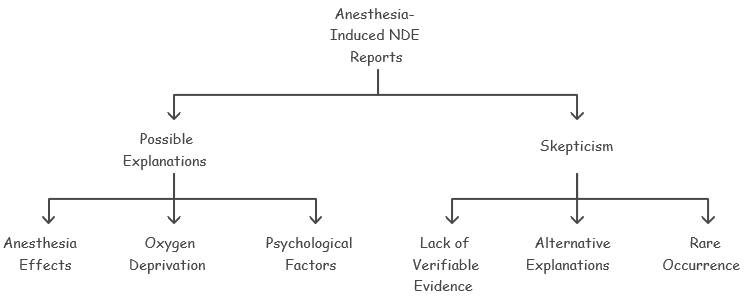
Here are some of the perspectives surrounding anesthesia-induced NDEs:
- Possible Explanations:
- Anesthesia Effects: Some researchers suggest that certain anesthetic drugs may induce hallucinations or dream-like states that could be mistaken for NDEs.
- Oxygen Deprivation: Brief periods of oxygen deprivation during surgery could potentially trigger altered states of consciousness similar to NDEs.
- Psychological Factors: The stress and anxiety surrounding surgery could contribute to the formation of unusual experiences upon waking.
- Skepticism:
- Lack of Verifiable Evidence: Many NDE accounts are subjective and difficult to verify objectively.
- Alternative Explanations: The experiences reported could often be explained by known physiological or psychological phenomena.
- Rare Occurrence: Anesthesia-induced NDEs are relatively rare, making it difficult to study systematically.
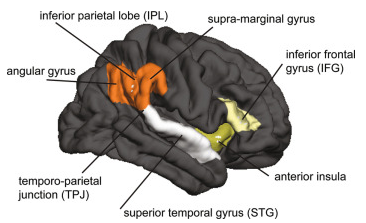
Are there any cases where stimulation of certain brain regions has induced experiences similar to Near-Death Experiences (NDEs) ?
Yes, there have been documented cases where stimulation of certain brain regions has induced experiences similar to Near-Death Experiences (NDEs)
- Temporo-Parietal Junction (TPJ) Stimulation: A patient undergoing treatment for epilepsy experienced an out-of-body experience (OBE) when the TPJ was electrically stimulated. The patient described sensations of floating above their body and viewing themselves from an external perspective. This area of the brain is involved in integrating sensory information and spatial awareness.
- Angular Gyrus Stimulation: Electrical stimulation of the angular gyrus led to OBEs in patients. They reported seeing themselves from an external vantage point and experiencing distortions in their perception of their body's position in space. The angular gyrus plays a role in processing spatial orientation and body perception.
- Right Temporal Lobe Stimulation: Using transcranial magnetic stimulation (TMS) on the right temporal lobe, participants reported experiences resembling NDEs, including feelings of a presence, floating sensations, and encountering bright lights. The right temporal lobe is associated with processing emotions and memory, which might explain these vivid experiences.
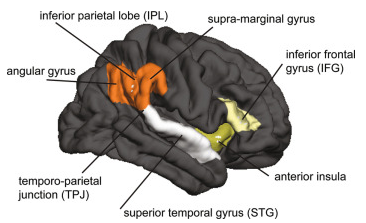
Image Source : Science Direct
These cases suggest that NDEs might not necessarily be linked to the dying process itself, but rather could be triggered by specific patterns of brain activity. The angular gyrus, in particular, has been implicated in several studies as playing a role in the experience of self-location and out-of-body sensations
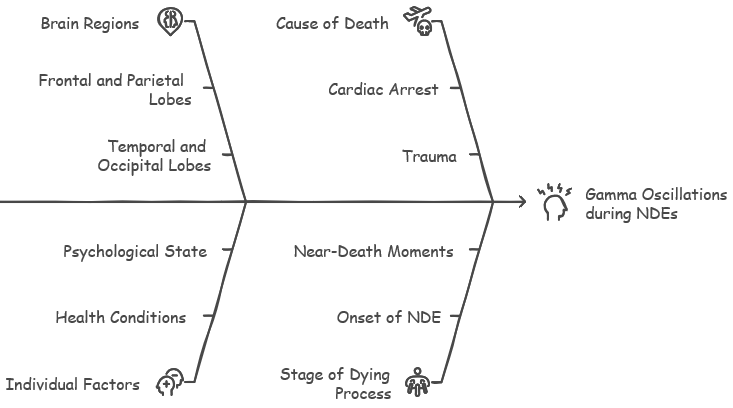
How gamma oscillation associated with any specific probe position can be explained in the context of NDE ?
In the context of NDE (neural dying process), gamma oscillations have been observed to increase during the dying process, not necessarily localized to a single probe position in the 10-20 EEG system. However, certain brain regions tend to show more pronounced gamma activity during this period.
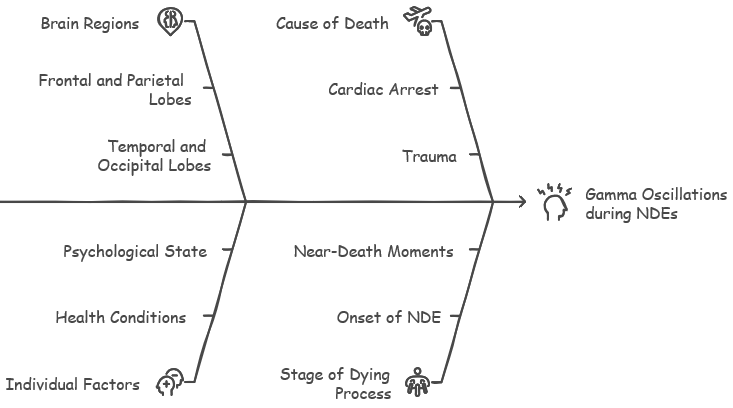
Common Regions Associated with Gamma Oscillations during NDE:
- Frontal and Parietal Lobes: These regions, associated with higher cognitive functions like attention, working memory, and perception, may show increased gamma oscillations during NDEs. This could be linked to the vivid and heightened experiences reported by some individuals, such as a sense of awareness, clarity, or a life review.
- Temporal Lobes: The temporal lobes, involved in auditory processing, memory formation, and emotional regulation, might also exhibit increased gamma activity during NDEs. This could relate to experiences of hearing voices, recalling memories, or feeling a sense of peace and tranquility.
- Occipital Lobes: While primarily associated with visual processing, increased gamma activity in the occipital lobes during NDEs could be linked to the perception of light or visions reported by some individuals.
Dynamic Nature of Gamma Oscillations during NDE:
The presence and intensity of gamma oscillations during the dying process can vary based on individual factors, the specific cause of death, and the stage of the dying process. Gamma activity might surge during specific moments, such as the onset of cardiac arrest or during a near-death experience.
Interpreting EEG Data in NDE Research:
While specific probe locations can offer valuable information about the distribution of gamma activity, it's essential to interpret EEG data in the context of the overall brain activity pattern during the dying process. Researchers often combine EEG recordings with other neuroimaging techniques and anecdotal reports to gain a more comprehensive understanding of the neural correlates of NDEs.
In conclusion, while gamma oscillations are not confined to a single probe position during NDEs, certain brain regions tend to exhibit more prominent gamma activity. Further research is needed to fully understand the complex and dynamic changes in brain activity during the dying process and their relationship to the subjective experiences reported by individuals who have had NDEs.
Yes, there are specific brain regions associated with consciousness that cease functioning at death. Consciousness is a complex and not fully understood phenomenon, but it is generally associated with a network of regions in the brain known as the "neural correlates of consciousness" (NCC). At the moment of death, brain activity ceases, and with it, the functioning of these critical regions linked to consciousness. This cessation includes a stop in electrical activity and the breakdown
of the biochemical processes necessary for these brain regions to function. This is why consciousness cannot continue once brain activity has stopped, marking the biological criterion for death.
- Cerebral Cortex:
- Frontal Lobe: This region is responsible for higher-order cognitive functions, such as reasoning, planning, decision-making, and self-awareness. Damage to the frontal lobe can lead to profound alterations in personality, behavior, and consciousness.
- Parietal Lobe: This area integrates sensory information from different modalities, creating a coherent perception of the world around us. It is also involved in attention, spatial awareness, and self-image. Dysfunction in the parietal lobe can result in distortions of body image, spatial neglect, and impaired consciousness.
- Thalamus:
- This structure acts as a central hub, relaying sensory information from the body to the cerebral cortex. It also plays a role in regulating sleep, wakefulness, and attention. Disruption of thalamic function can lead to coma and loss of consciousness.
- Brainstem:
- Reticular Activating System (RAS): This network of neurons within the brainstem is responsible for maintaining arousal and wakefulness. It modulates the level of consciousness and attention. Damage to the RAS can result in coma or other disorders of consciousness.
- Other Brainstem Structures: The brainstem also houses vital centers for controlling breathing, heart rate, and other essential bodily functions. These functions are necessary for sustaining life and, indirectly, consciousness.
- Additional Considerations:
- Connectivity: Consciousness is not localized to a single brain region but arises from the complex interaction and communication between multiple brain areas. The coordinated activity of these regions, facilitated by neural networks, is crucial for conscious experience.
- Integrated Information Theory (IIT): This theory proposes that consciousness is a fundamental property of integrated information within a system. According to IIT, the level of consciousness depends on the amount and complexity of information integrated across the brain.
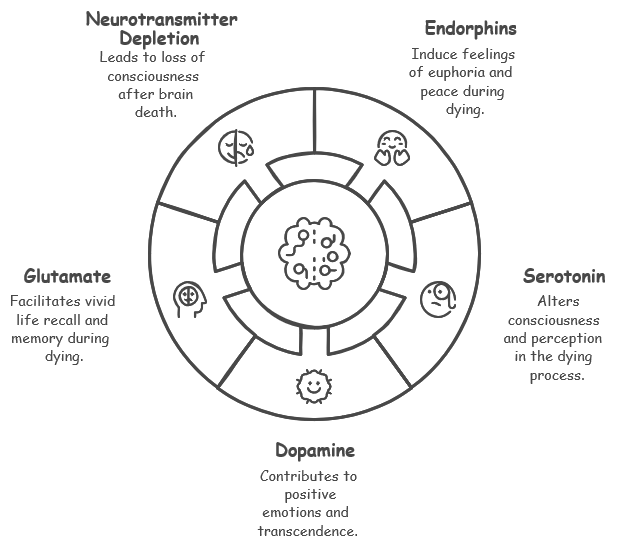
Neurotransmitters play a significant, yet complex, role in the experience of dying. Overall, the role of neurotransmitters in the experience of dying is complex and not fully understood. Research suggests that they likely contribute to the subjective experiences reported by some individuals, such as feelings of peace, euphoria, and hallucinations. However, the exact mechanisms and interactions of neurotransmitters during this process remain an area of active investigation.
Additionally, it's important to note that the experience of dying is highly individual and can be influenced by various factors, including cultural beliefs, personal experiences, and the underlying cause of death. Followings are a list of Neurotransmitters that are considered to be involved in dying process :
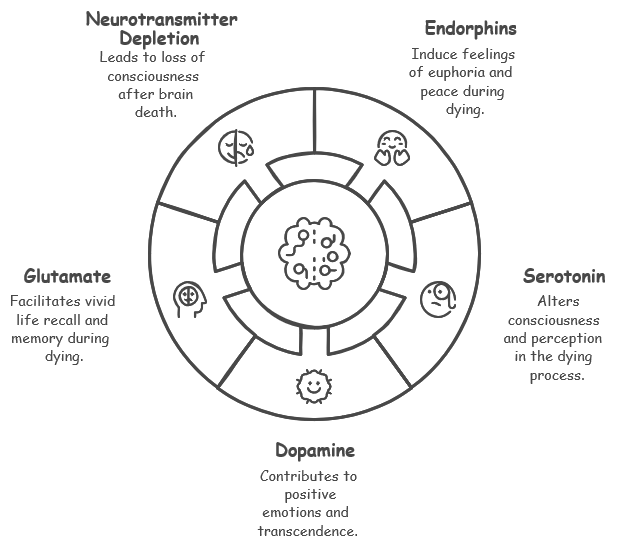
- During the dying process:
- Endorphins: These natural painkillers and mood elevators are released in response to stress and pain. They can induce feelings of euphoria, peace, and detachment, which may contribute to the positive experiences reported by some individuals near death.
- Serotonin: This neurotransmitter regulates mood, sleep, and perception. Fluctuations in serotonin levels during the dying process could potentially explain the altered states of consciousness and hallucinations reported in some cases.
- Dopamine: Involved in reward, motivation, and pleasure, dopamine release could also contribute to the positive emotions and feelings of transcendence sometimes associated with near-death experiences.
- Glutamate: This excitatory neurotransmitter plays a crucial role in learning and memory. A surge in glutamate levels during the dying process has been hypothesized to contribute to the vivid recall of life events or the "life review" phenomenon reported by some individuals.
- After brain death:
- Neurotransmitter depletion: As brain function ceases, neurotransmitter levels gradually decrease. This depletion contributes to the loss of consciousness and the cessation of all cognitive and sensory experiences.
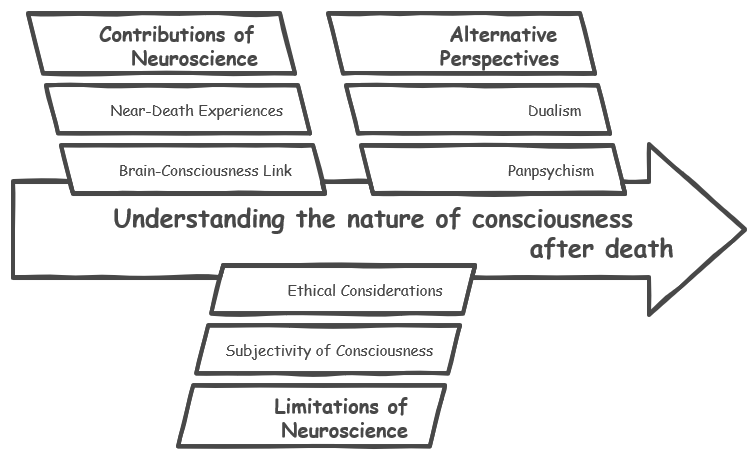
Neuroscience offers valuable insights into the relationship between the brain and consciousness, but its ability to definitively shed light on the nature of consciousness after death is limited. While neuroscience can offer valuable insights into the relationship between the brain and consciousness, it cannot definitively answer the question of consciousness after death. The nature of consciousness remains a complex and elusive topic, with ongoing research exploring its neural correlates and
potential implications beyond the physical brain.
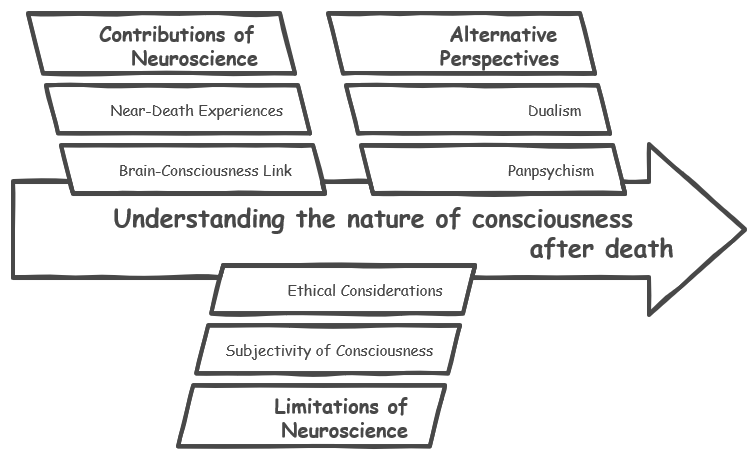
- Constributions of Neuroscience :
- Brain-Consciousness Link: Neuroscience has established a strong correlation between brain activity and consciousness. When specific brain regions cease to function, consciousness is lost. This suggests that consciousness may be dependent on a functioning brain.
- Near-Death Experiences (NDEs): Studying NDEs can provide clues about how the brain generates conscious experiences during extreme conditions. While NDEs are often interpreted as evidence of consciousness beyond death, neuroscience research suggests they could be explained by neurological processes occurring in a dying brain.
- Brain Activity After Death: Recent studies have detected bursts of brain activity, such as gamma waves, in some individuals after clinical death. While this raises questions about the possibility of residual consciousness, it doesn't necessarily prove its existence beyond the brain's cessation.
- Limitations of Neuroscience:
- Subjectivity of Consciousness: Consciousness is a subjective experience, making it difficult to measure and study objectively using neuroscientific tools.
- Ethical Considerations: Studying consciousness during the dying process raises ethical concerns regarding patient consent and potential harm.
- Lack of Evidence: There is no definitive scientific evidence supporting the existence of consciousness independent of the brain.
- Alternative Perspectives:
- Dualism: This philosophical view posits that consciousness and the brain are separate entities. While dualism allows for the possibility of consciousness surviving death, it lacks empirical evidence from neuroscience.
- Panpsychism: This theory suggests that consciousness is a fundamental property of the universe and exists in various forms, even in inanimate objects. However, panpsychism is more of a philosophical concept and not directly supported by neuroscientific findings.
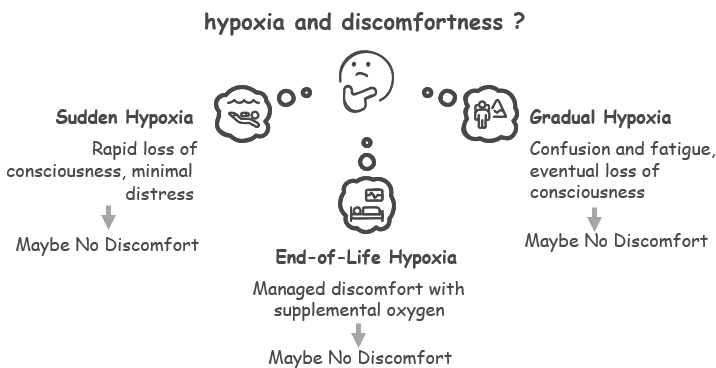
The sensation of extreme discomfort and air hunger experienced when holding one's breath is primarily due to the buildup of carbon dioxide (CO2) in the body, rather than the lack of oxygen itself. This triggers a physiological response, including increased heart rate, panic, and the urge to breathe.
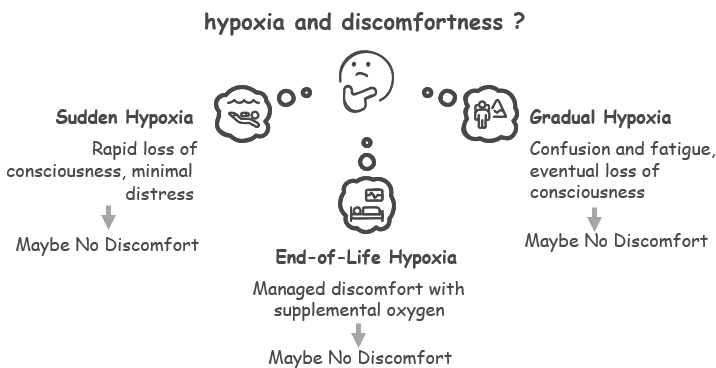
In contrast, the experience of dying from oxygen deprivation (hypoxia) can vary significantly depending on the specific circumstances:
- Sudden Hypoxia: In cases of sudden and complete oxygen deprivation, such as drowning or suffocation, consciousness is lost rapidly, often before the individual can experience significant distress.
- Gradual Hypoxia: In situations where oxygen levels decrease gradually, such as in certain medical conditions or high-altitude environments, the individual may experience symptoms like confusion, dizziness, fatigue, and eventually, loss of consciousness. However, the intense air hunger associated with holding one's breath may not be present.
- End-of-Life Hypoxia: In the context of dying from a terminal illness or organ failure, oxygen deprivation may occur gradually. Patients are often provided with supplemental oxygen and medications to manage discomfort and distress.
Furthermore, the release of endorphins and other neurotransmitters during the dying process could potentially mask or alter the perception of pain and discomfort.
Therefore, while the urge to breathe and air hunger experienced when holding one's breath are primarily driven by CO2 buildup, the sensation of dying from oxygen deprivation is more complex and variable. It can depend on the rate of oxygen depletion, individual factors, and the presence of other physiological responses.
Medically assisted dying (MAID), from a neurological perspective, can be understood as a process aimed at inducing a peaceful and irreversible loss of consciousness and brain function. The medications used in MAID typically target specific neurotransmitter systems to achieve this goal.
The most common medications used in MAID are:
- Barbiturates: These drugs act on the GABAergic system, the brain's primary inhibitory neurotransmitter system. By enhancing GABA's inhibitory effects, barbituratessuppress neuronal activity throughout the brain, leading to loss of consciousness, respiratory depression, and ultimately, cessation of brain function.
- Neuromuscular Blocking Agents: These drugs are sometimes used in conjunction with barbiturates to induce muscle relaxation and paralysis. They work by blocking the transmission of signals between nerves and muscles, preventing muscle contractions and ensuring a peaceful death.
Neurological Effects of these medications are :
- Loss of Consciousness: The primary aim of MAID is to rapidly induce a deep and irreversible coma, resulting in the loss of consciousness and awareness.
- Suppression of Brain Activity: The medications used in MAID suppress electrical activity throughout the brain, including the regions responsible for consciousness, sensation, and thought.
- Respiratory Depression: Barbiturates depress the respiratory centers in the brainstem, leading to the cessation of breathing.
- Cardiac Arrest: Following respiratory arrest, the heart eventually stops beating due to lack of oxygen, resulting in death.
It is important to note that while MAID aims to provide a peaceful and painless death, the exact neurological mechanisms underlying the loss of consciousness and cessation of brain function are complex and not fully understood.
Followings are some specific examples of the medication for MAID based on Medical assistance in dying (MAiD) PINs
Following is the list of medications and description for a Intravenous Kit
|
Medication
|
Effect in MAID
|
|
Lidocaine 1% injection
|
Used to numb specific areas of the body to minimize pain from the administration of other injectable medications.
|
|
Lidocaine 2% injection
|
Similar use as Lidocaine 1%, providing local anesthesia to manage pain at the injection site.
|
|
Bupivacaine 5 mg/mL injection
|
Long-acting local anesthetic used to manage pain at the injection site.
|
|
Midazolam 1 mg/mL injection
|
Used for sedation to reduce anxiety and induce sedation, making the process more comfortable for the patient.
|
|
Midazolam 5 mg/mL injection
|
Higher dosage of Midazolam, enhances sedative effects to ensure comfort and calm during the procedure.
|
|
Phenobarbital Sodium 120 mg/mL injection
|
Barbiturate that induces deep sedation or coma, leading to cessation of brain activity and respiratory arrest.
|
|
Propofol 10 mg/mL injection
|
Induces a deep, painless unconscious state before administering drugs that lead to cessation of life functions.
|
|
Rocuronium Bromide 10 mg/mL injection
|
Muscle relaxant used to ensure no physical signs of discomfort or convulsions as death approaches.
|
|
Sodium Chloride 0.9% injection
|
Used as a diluent or carrier for other medications to ensure efficient delivery into the bloodstream.
|
Following is the list of medications and description for an Oral Kit
|
Medication
|
Effect in MAID
|
|
Haloperidol 5 mg/mL injection
|
Used primarily to control symptoms like agitation or delirium. It helps in calming the patient.
|
|
Lorazepam 0.5 mg SL tablet
|
Sublingual lorazepam is effective for reducing anxiety and providing sedation, ensuring the patient remains calm and comfortable.
|
|
Metoclopramide 10 mg tablet
|
Used to prevent nausea and vomiting, which can be side effects of other drugs used in MAID.
|
|
Ondansetron 8 mg tablet
|
Another antiemetic, ondansetron is used to control nausea and vomiting from other medications or the condition itself.
|
|
Phenobarbital + chloral hydrate + morphine sulphate oral suspension
|
This combination is used for its sedative, hypnotic, and analgesic properties to manage pain, induce sleep, and reduce awareness.
|
|
Secobarbital compound suspension
|
Secobarbital is a potent barbiturate used to induce deep sedation or coma rapidly, leading to cessation of life functions.
|
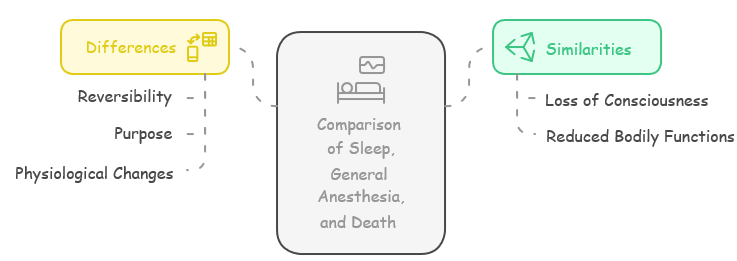
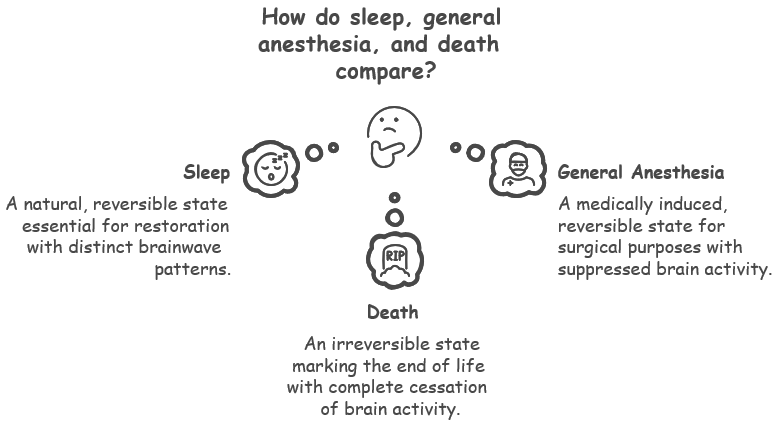
Sleep, general anesthesia, and death are distinct states with some similarities and key differences. Sleep, general anesthesia, and death share some similarities in terms of loss of consciousness and reduced bodily functions. However, their reversibility, purpose, and specific physiological changes distinguish them as fundamentally different states.
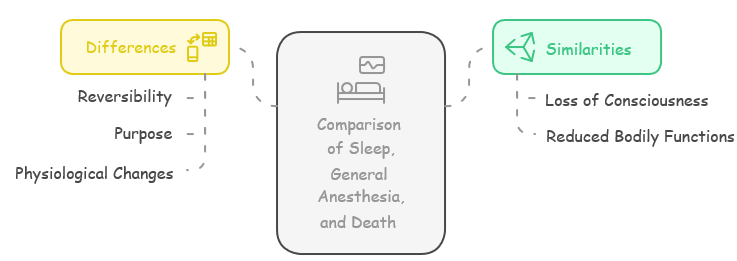
What are Similarities ?
Sleep, general anesthesia, and death might seem very different, but they have some interesting things in common. All three change how aware we are and affect our bodies in similar ways. Even though they last for different amounts of time and happen for different reasons, each one shows us how delicate the balance is between being alive, being unconscious, and not being alive anymore. By looking at what sleep, general anesthesia, and death share, we can better understand how our bodies work
and the mysteries that scientists and thinkers are still trying to figure out.
Followings are key similarities:
- Loss of consciousness: All three involve a loss of awareness and responsiveness to the environment.
- Reduced bodily functions: Heart rate, breathing, and other bodily functions slow down in all three states.
What are key differences:
Even though sleep, general anesthesia, and death all make us unconscious, they are actually very different. Sleep is like taking a break each night, and we always wake up feeling refreshed. General anesthesia is like being put to sleep for surgery, and doctors make sure we wake up safely. But death is permanent—it's the end of life. They also have different purposes, last for different amounts of time, and affect our bodies in unique ways. By looking closely at these differences, we can learn
more about how our bodies work and the important things that separate being alive, being temporarily unconscious, and being dead.
Followings are key differences :
- Reversibility: Sleep and general anesthesia are reversible states. Individuals awaken from sleep naturally or with external stimuli, while general anesthesia is reversed by stopping the medication. Death, however, is irreversible.
- Purpose: Sleep is a natural restorative process essential for physical and mental well-being. General anesthesia is medically induced to facilitate surgery or other procedures. Death is the cessation of life.
- Physiological changes: While all three states involve changes in brain activity, the specific patterns differ. Sleep has distinct stages with varying brainwave patterns, while general anesthesia aims to suppress brain activity. Death involves the complete cessation of brain activity.
How do you compare the three status in terms of brain wave ?
Sleep, general anesthesia, and death all have distinct effects on brain wave patterns, reflecting the different states of consciousness and neural activity associated with each. While all three states involve alterations in brain wave patterns, the specific changes differ significantly. Sleep demonstrates a cyclical pattern of varying brain wave activity, general anesthesia suppresses brain waves to induce unconsciousness, and death marks the complete cessation of brain wave activity.
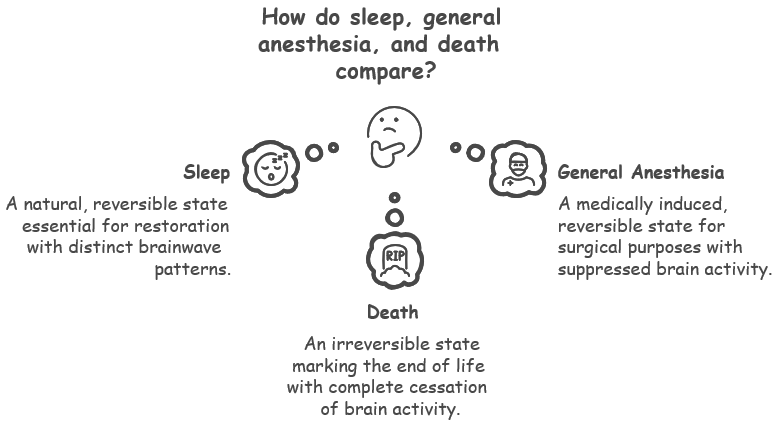
- Sleep:
- Brain wave patterns change throughout the different sleep stages.
- Non-REM sleep: Characterized by slower brain waves (theta and delta waves) as sleep deepens.
- REM sleep: Brain wave patterns become more similar to wakefulness (faster beta waves), and this is when most dreaming occurs.
- General Anesthesia:
- Aims to suppress brain activity to induce unconsciousness.
- Initially, there might be a brief period of increased brain wave activity.
- As anesthesia deepens, brain waves slow down significantly, with a predominance of delta and theta waves.
- Different anesthetic drugs can produce slightly different patterns.
- Death:
- Brain wave activity ceases entirely.
- There might be a brief surge of activity right before or after the heart stops, but this is not sustained.
- This flatlining of brain waves is a key indicator of brain death.
Reference
YouTube
|
|